Get Started
Research Guides
A Place to Start
Choose a tutorial or guide to kickstart your research
A-Z Database List
FIND A Database
Search 130+ databases for research and articles
Borrowing
Check it
Out
Check out books, models, hotspots and more
Print, Copy & Scan
Ready to Print
Add funds, install drivers, use mobile printing
Search Our Catalog
Find articles, journals, e-books & more using our online library catalog.
Library CatalogeBookseJournals/Articles
Find an article using one of the databases in the drop-down menu
Not sure where to start? Try one of our favorites below!
Search for E-Journals
Search for E-Books & More
Search for items in the UNTHSC Scholarly Repository
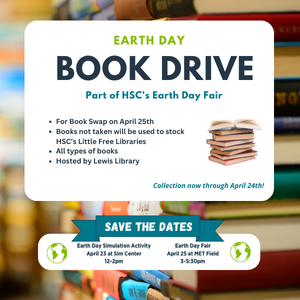
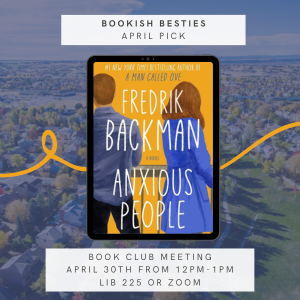
Upcoming Events
Apr 30, 2024
12:00 pm – 1:00 pm
April Bookish Besties Meeting
LIB-225 & Zoom
Bookish Besties Book Club